Drew Scott's Illness: Understanding Transverse Myelitis + His Story
Ever wondered about the health battles even celebrities face behind the glitz and glamour? Drew Scott, the charismatic co-host of "Property Brothers," faced a significant health challenge, battling a rare autoimmune disease.
Drew Scott, widely recognized as one half of the dynamic duo from the home renovation hit "Property Brothers," received a diagnosis of transverse myelitis in 2015. This diagnosis brought to light a condition that, while rare, can have profound effects on those affected. Transverse myelitis is characterized by inflammation of the spinal cord, leading to damage of nerve fibers and subsequent neurological deficits. This inflammation disrupts the communication between the brain and the rest of the body, potentially resulting in a range of symptoms that impact motor and sensory functions. Symptoms can manifest as muscle weakness, paralysis affecting the legs, arms, or trunk, sensory abnormalities like numbness or tingling sensations in the extremities, and issues with bowel and bladder control, reflecting the diverse roles the spinal cord plays in bodily functions.
Following his diagnosis, Drew Scott engaged in a comprehensive treatment plan that included high-dose steroid therapy to reduce inflammation and intensive physical therapy to regain strength and mobility. While Scott has made significant progress, recovering much of his previous functionality, he has acknowledged experiencing some residual weakness in his legs. Scott's openness about his health journey has been instrumental in increasing awareness of transverse myelitis, providing a platform for education and support for others navigating the same condition.
- Danny Duncan Net Worth 2024 Wie Viel Verdient Er Wirklich
- John Oates Vermgen 2023 So Reich Ist Er Wirklich Geheimnisse
Although transverse myelitis presents significant challenges, it's important to recognize that it is a treatable condition. Early intervention and appropriate medical management can greatly improve outcomes, allowing many individuals to recover a considerable degree of function and maintain a good quality of life. The key lies in prompt diagnosis and tailored treatment strategies to minimize the impact of the disease on the spinal cord.
| Category | Information |
|---|---|
| Name | Drew Scott |
| Born | April 28, 1978 |
| Occupation | Television personality, Real Estate Investor, Author, Producer, and Entrepreneur |
| Known For | Co-hosting "Property Brothers" alongside his twin brother Jonathan Scott |
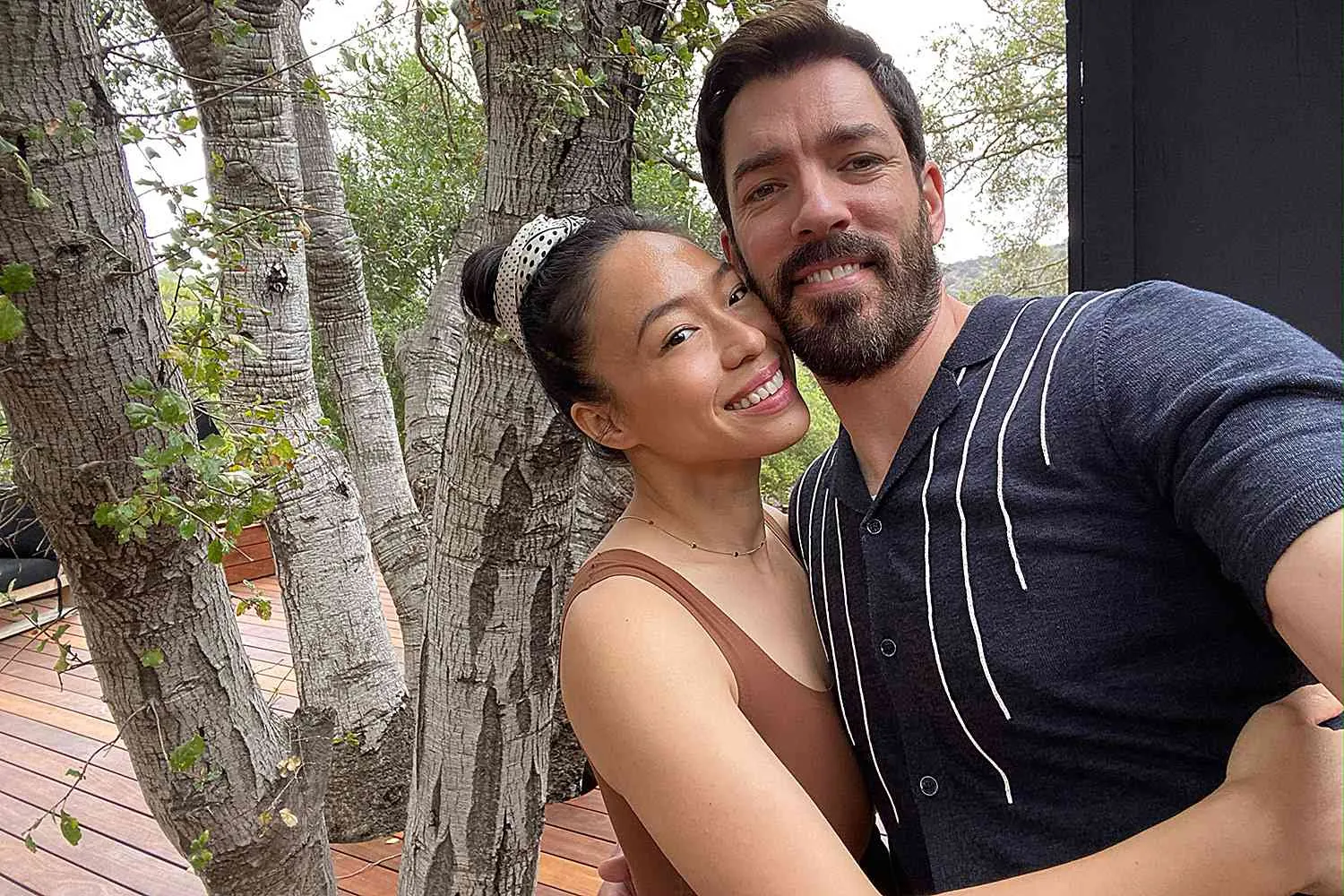
| Spouse | Linda Phan (married in 2018) |
| Children | Parker James Scott (born May 2022) |
| Diagnosis Date | 2015 |
| Illness | Transverse Myelitis |
| Treatment | Steroids, Physical Therapy |
| Website | Scott Brothers Entertainment |
Transverse myelitis, the condition Drew Scott faced, is a rare inflammatory disorder affecting the spinal cord. The exact cause often remains elusive, but when it strikes, the consequences can be far-reaching. It's a neurological condition where inflammation disrupts the normal function of the spinal cord, which serves as the critical link between the brain and the rest of the body. As a result, individuals may experience motor, sensory, and autonomic dysfunction. While it's not a commonly discussed ailment, its impact on those affected is significant, making awareness and understanding paramount. The inflammation characteristic of transverse myelitis can damage or destroy the myelin sheath, the protective covering around nerve fibers. This damage disrupts the transmission of nerve signals, leading to a variety of neurological symptoms. The severity and nature of these symptoms depend on the extent and location of the inflammation in the spinal cord.
- Definition: Transverse myelitis is a rare autoimmune disease that affects the spinal cord, leading to inflammation and neurological dysfunction.
- Symptoms: Symptoms can vary widely but commonly include weakness, paralysis, numbness, tingling, and bowel or bladder dysfunction.
- Diagnosis: Diagnosis typically involves a physical exam, medical history review, and diagnostic tests like MRI scans and spinal taps to confirm the condition.
- Treatment: Treatment focuses on reducing inflammation and managing symptoms, often including steroids, physical therapy, and occupational therapy.
- Prognosis: The prognosis varies depending on the severity and individual response to treatment, with some experiencing full recovery and others facing permanent disability.
Drew Scott's decision to share his battle with transverse myelitis has brought much-needed attention to this relatively unknown condition. By sharing his personal experiences, he not only demystifies the illness but also provides hope and encouragement to others who are facing similar health challenges. Scott's openness reinforces the importance of support networks, including family, friends, and healthcare professionals, in navigating the physical and emotional toll of chronic illness. His determination to live a full and active life despite his diagnosis serves as an inspiration to many, highlighting the resilience of the human spirit.
- Hat Wentworth Miller Wirklich Eine Familie Das Steckt Dahinter
- Kevin Durants Frau Wahrheit Amp Gerchte Um Kevin Durant Frau
The core of the issue lies in the spinal cord, the body's information superhighway. Inflammation there can disrupt the signals traveling to and from the brain, causing a cascade of problems. Imagine a traffic jam on a major highway thats essentially whats happening in the spinal cord during a transverse myelitis episode.
- Causes: The causes of transverse myelitis are diverse and often elusive. It can be triggered by viral or bacterial infections, autoimmune disorders like multiple sclerosis or lupus, or as a rare reaction to vaccinations. In some cases, the cause remains unknown, termed idiopathic transverse myelitis.
- Symptoms: Symptoms manifest differently from person to person but commonly include weakness in the arms and legs, sensory changes such as numbness, tingling, or burning sensations, and bowel and bladder dysfunction. These symptoms may develop rapidly over hours or days, or gradually over weeks.
- Diagnosis: Diagnosing transverse myelitis involves a comprehensive approach. Neurological examinations assess motor and sensory functions, while magnetic resonance imaging (MRI) of the spinal cord helps visualize inflammation or other abnormalities. A spinal tap, or lumbar puncture, may be performed to analyze cerebrospinal fluid for signs of infection or inflammation.
- Treatment: The primary goals of treatment are to reduce inflammation and alleviate symptoms. Corticosteroids, administered intravenously or orally, are often used to suppress the immune system and decrease inflammation. Physical therapy and occupational therapy play a crucial role in regaining strength, improving coordination, and adapting to any residual deficits. In some cases, antiviral medications or plasma exchange therapy may be considered.
Drew Scott's experience underscores the reality that even those in the public eye are not immune to health challenges. His willingness to share his journey has not only increased awareness of transverse myelitis but has also demonstrated the importance of early diagnosis and treatment in managing the condition effectively. It highlights the crucial role of support networks and the ability of individuals to maintain an active and fulfilling life despite chronic illness. His advocacy empowers others to seek timely medical care and engage in proactive self-management strategies.
The range of experiences with transverse myelitis is vast, from those who recover completely to those who face long-term challenges. It highlights the importance of individualized care and the understanding that each person's journey is unique. The key is to address the inflammation swiftly and to implement a rehabilitation plan that focuses on regaining lost function and maximizing independence.
The effects of transverse myelitis are varied and depend on the individual and the severity of the inflammation. While some individuals experience mild, temporary symptoms, others face significant, long-lasting disability. Understanding these varied outcomes is essential for setting realistic expectations and providing appropriate support.
- Weakness or paralysis in the legs, arms, or trunk: This is a hallmark symptom of transverse myelitis, resulting from the disruption of motor pathways in the spinal cord. The degree of weakness or paralysis can range from mild difficulty with movement to complete loss of motor function. It may affect one or both sides of the body, depending on the location and extent of the spinal cord inflammation.
- Numbness or tingling in the extremities: Sensory changes are common in transverse myelitis, reflecting the involvement of sensory pathways in the spinal cord. Individuals may experience numbness, tingling, burning sensations, or heightened sensitivity to touch. These sensory abnormalities can affect the hands, feet, legs, or arms, and may be accompanied by pain.
- Difficulty with bowel and bladder function: The spinal cord plays a crucial role in controlling bowel and bladder function, and inflammation can disrupt these processes. Individuals with transverse myelitis may experience urinary retention, urinary incontinence, constipation, or fecal incontinence. These bowel and bladder symptoms can significantly impact quality of life and require careful management.
Drew Scott's experience illuminates the impact of transverse myelitis on daily life, emphasizing the importance of seeking timely medical attention and engaging in rehabilitation. His story serves as a reminder that chronic illness can affect anyone, regardless of their public persona, and that early intervention can improve outcomes. It reinforces the need for increased awareness and understanding of rare conditions like transverse myelitis.
Reaching a diagnosis of transverse myelitis requires a thorough and multifaceted approach. The process begins with a detailed neurological examination to assess motor and sensory functions, followed by a review of the patient's medical history to identify any potential risk factors or underlying conditions.
- Physical examination: A comprehensive physical examination is essential for identifying the characteristic signs of transverse myelitis, such as muscle weakness, sensory changes, and bowel or bladder dysfunction. The examination helps determine the extent and severity of neurological deficits, guiding further diagnostic evaluations.
- Medical history: A thorough review of the patient's medical history can uncover potential causes or contributing factors to transverse myelitis, such as recent infections, autoimmune disorders, or vaccinations. Identifying any underlying medical conditions is crucial for guiding treatment strategies.
- MRI scan: Magnetic resonance imaging (MRI) of the spinal cord is a key diagnostic tool for visualizing inflammation or other abnormalities. The MRI scan helps confirm the diagnosis of transverse myelitis and rule out other potential causes of spinal cord dysfunction, such as tumors or compression.
- Spinal tap: A spinal tap, or lumbar puncture, involves collecting a sample of cerebrospinal fluid (CSF) for analysis. CSF analysis can help identify signs of infection, inflammation, or other abnormalities that may be contributing to transverse myelitis. It also helps rule out other conditions, such as meningitis or encephalitis.
Drew Scott's experience highlights the importance of a meticulous diagnostic process in cases of suspected transverse myelitis. His story emphasizes the need for healthcare professionals to consider rare conditions and to utilize a combination of clinical evaluation and diagnostic testing to reach an accurate diagnosis. It underscores the value of patient advocacy in ensuring timely and appropriate medical care.
Management of transverse myelitis is a multifaceted undertaking, aimed at reducing inflammation, managing symptoms, and maximizing functional recovery. Drew Scott's experience underscores the significance of a comprehensive treatment strategy tailored to the individual's specific needs.
- Steroids: Steroids, such as corticosteroids, are frequently used to reduce inflammation in the spinal cord. They are typically administered intravenously (IV) in high doses for a limited period to suppress the immune system and alleviate symptoms.
- Physical therapy: Physical therapy plays a vital role in regaining strength, improving range of motion, and enhancing coordination. Therapists work with individuals to develop personalized exercise programs that target specific muscle groups affected by transverse myelitis.
- Occupational therapy: Occupational therapy focuses on improving activities of daily living, such as dressing, bathing, and eating. Occupational therapists help individuals adapt to any functional limitations and provide assistive devices or strategies to promote independence.
Drew Scott's journey highlights the collaborative approach to treatment, involving a team of doctors, nurses, and therapists. It emphasizes the importance of patient education and self-management strategies in optimizing outcomes and improving quality of life. It serves as an inspiration to others facing similar health challenges.
The long-term outlook for individuals with transverse myelitis varies significantly, depending on the severity of the initial inflammation and the individual's response to treatment. While some individuals experience a full recovery, others may face ongoing challenges.
The extent of damage to the spinal cord is a critical factor in determining the long-term prognosis. Individuals with mild cases of transverse myelitis may experience temporary weakness or numbness that resolves with treatment. However, those with more severe cases may face permanent paralysis or other disabilities.
Drew Scott's relatively mild case of transverse myelitis and his subsequent recovery offer hope and encouragement to others facing similar diagnoses. His story underscores the importance of early intervention and the potential for positive outcomes with appropriate medical care and rehabilitation. It emphasizes the resilience of the human spirit and the ability to overcome health challenges.
While there is no cure for transverse myelitis, effective treatments are available to manage symptoms and prevent further damage to the spinal cord. These treatments include steroids, physical therapy, and occupational therapy. The overall prognosis varies depending on the individual's response to treatment and the severity of the initial inflammation.
Drew Scott's experience serves as a reminder of the importance of a multidisciplinary approach to managing transverse myelitis, involving doctors, nurses, and therapists. It highlights the need for individualized treatment plans that address each patient's specific needs and goals. It emphasizes the value of ongoing support and encouragement throughout the recovery process.
Transverse myelitis is a complex condition, and many questions arise for those affected and their loved ones. Understanding the nuances of this illness is essential for navigating the challenges it presents. Here are some frequently asked questions, offering clarity and guidance.
Question 1: What exactly is transverse myelitis?
Transverse myelitis is a rare neurological disorder characterized by inflammation of the spinal cord. This inflammation disrupts the normal transmission of nerve signals between the brain and the rest of the body, leading to a range of symptoms, including weakness, sensory changes, and bowel or bladder dysfunction. It is considered an autoimmune condition, as the immune system mistakenly attacks the spinal cord.
Question 2: What are the telltale symptoms of transverse myelitis?
The symptoms of transverse myelitis can vary widely, depending on the severity of the inflammation and the location of the affected area in the spinal cord. Some individuals may experience only mild symptoms, such as localized numbness or tingling, while others may face severe symptoms that significantly impact their daily lives. Common symptoms include muscle weakness, paralysis, sensory changes (numbness, tingling, burning sensations), and bowel or bladder dysfunction.
Question 3: How does a doctor diagnose transverse myelitis?
Diagnosing transverse myelitis involves a comprehensive approach that includes a thorough physical examination, a review of the patient's medical history, and various diagnostic tests. An MRI scan of the spinal cord is crucial for visualizing inflammation or other abnormalities. A spinal tap, or lumbar puncture, may be performed to analyze cerebrospinal fluid for signs of infection or inflammation.
Question 4: What are the available treatment options for transverse myelitis?
While there is no definitive cure for transverse myelitis, treatment aims to reduce inflammation, manage symptoms, and prevent further damage to the spinal cord. Corticosteroids are often used to suppress the immune system and decrease inflammation. Physical therapy and occupational therapy play essential roles in regaining strength, improving coordination, and adapting to any residual deficits.
Question 5: What does the future hold for someone with transverse myelitis?
The prognosis for transverse myelitis varies depending on the severity of the condition and the individual's response to treatment. Some individuals make a full recovery, while others experience permanent disability. Factors such as the extent of spinal cord damage and the presence of underlying medical conditions can influence the long-term outlook.
Question 6: What can we learn from Drew Scott's journey with transverse myelitis?
Drew Scott's experience with transverse myelitis sheds light on the challenges and triumphs of living with a rare autoimmune disease. His openness about his diagnosis has raised awareness of the condition and inspired others facing similar health battles. His story underscores the importance of early diagnosis, comprehensive treatment, and ongoing support in managing transverse myelitis effectively.
Transverse myelitis is a serious but manageable condition that can affect the spinal cord. The severity of symptoms can vary, and while there is no cure, treatments can help improve outcomes. Drew Scott's experience reminds us that even rare illnesses can be overcome with proper care and support.
Continue learning about transverse myelitis and related autoimmune diseases for a deeper understanding of these conditions.
Drew Scott's battle with transverse myelitis serves as a potent reminder of the challenges posed by rare autoimmune conditions. His story has not only heightened awareness but also provided inspiration and hope for those grappling with similar health issues.
Scott's journey highlights the critical role of early diagnosis, comprehensive treatment, and unwavering support in managing transverse myelitis effectively. His advocacy has empowered countless individuals to seek timely medical care and actively participate in their own recovery.
Transverse myelitis remains a complex condition, but advancements in medical knowledge and treatment options offer renewed hope for those affected. With dedicated care and support, individuals with transverse myelitis can lead fulfilling and active lives.
Article Recommendations


Detail Author:
- Name : Prof. Friedrich Kessler
- Username : skylar.jenkins
- Email : schmitt.ralph@hotmail.com
- Birthdate : 2001-07-10
- Address : 35096 Ratke Drive Apt. 031 Reynoldston, ME 12506-3024
- Phone : 432-443-4582
- Company : Bins Group
- Job : Nuclear Engineer
- Bio : Omnis aliquid dolores est libero asperiores libero nemo. Eum autem rem similique. Ut impedit repudiandae commodi.
Socials
tiktok:
- url : https://tiktok.com/@anna.cartwright
- username : anna.cartwright
- bio : Hic est sed repudiandae earum neque error nulla reprehenderit.
- followers : 556
- following : 2888
linkedin:
- url : https://linkedin.com/in/anna_cartwright
- username : anna_cartwright
- bio : Corrupti fugiat quo assumenda voluptas vitae.
- followers : 4115
- following : 810
facebook:
- url : https://facebook.com/anna_real
- username : anna_real
- bio : Esse sint nam maiores et. Quia occaecati aut quos maiores.
- followers : 5795
- following : 1844